About Kidney Health
Chronic Kidney Disease (CKD)
Most people don’t realize how kidneys work or what happens when they fail.
Chronic Kidney Disease (CKD) can progress to kidney failure (also called end-stage kidney disease), when less than 15% of kidney function remains. Below 10%, dialysis or a kidney transplant is often needed.

What Causes Kidney Damage?
Each kidney has about a million filters (nephrons). Some cells, like podocytes, cannot regenerate. Podocytes prevent important proteins (like albumin) from leaking into urine. Albumin in urine (albuminuria) is an early sign of damage and should be monitored.
When some nephrons are lost, others work harder, increasing pressure to keep up function. This can lead to further damage and more albumin loss. Over time, this overwork causes irreversible decline and can lead to kidney failure.
Why Early Detection Matters
Kidney damage also affects the heart and blood vessels, leading to Cardiovascular-Renal-Metabolic Syndrome. This shows how closely CKD, heart disease, and diabetes are linked. Detecting and treating CKD early helps protect overall health.
Signs and Detection
- Early stages often show no symptoms. Damage is only found by checking urine for albumin and blood for creatinine.
- Later symptoms (when function <30%) include:
- High blood pressure
- Fatigue
- Fluid retention
- Nausea
- Itching
- Reduced appetite or energy
Unfortunately, many people only learn they have kidney failure when they suddenly need dialysis. In 30% of cases, dialysis starts as an emergency.
5 Stages of Chronic Kidney Disease CKD
CKD is defined as abnormalities of kidney structure or function, present for a minimum of 3 months, with implications for health. CKD is classified via five stages based on Cause, Glomerular filtration rate (GFR) category (G1–G5), and Albuminuria category (A1–A3), abbreviated as CGA (see Table below > and this link is useful for explaining the table).
Stratification of the risk of CKD progression
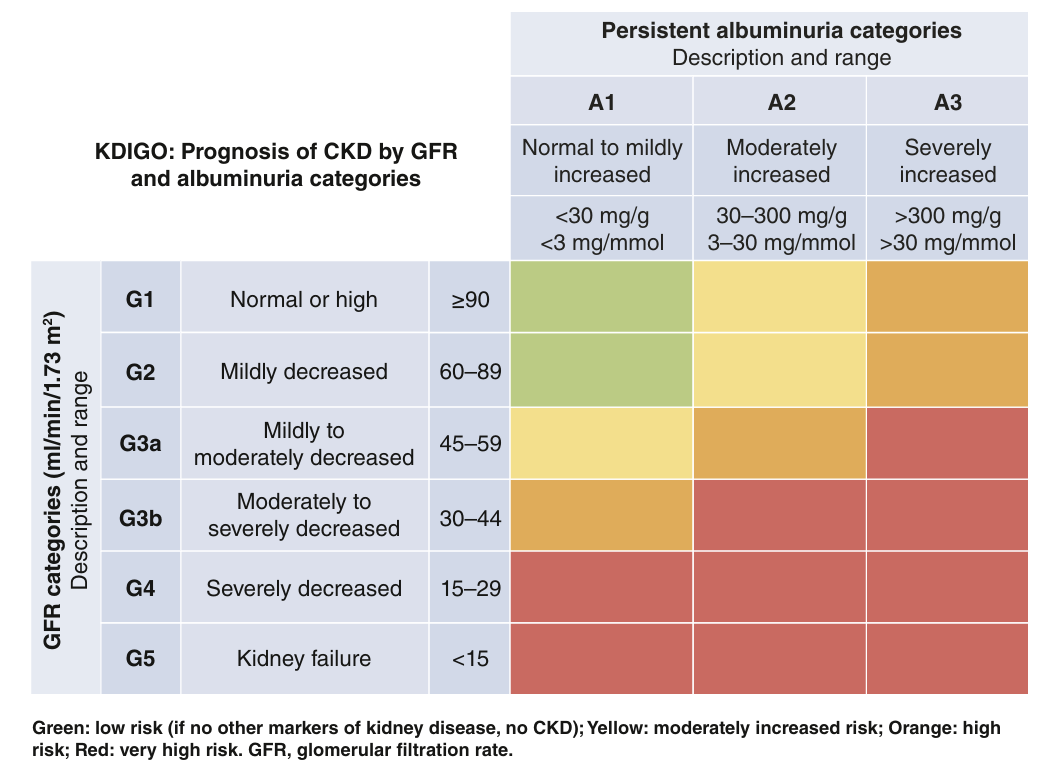
KDIGO 2024 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease VOLUME 105 | ISSUE 4S | APRIL 2024 https://kdigo.org/wp-content/uploads/2024/03/KDIGO-2024-CKD-Guideline.pdf

Complications and Causes of Chronic Kidney Disease (CKD)
Life with Kidney Failure
When kidney function drops below 5–10 ml/min (very severe failure), Kidney Replacement Therapy (KRT)—dialysis or transplant—is needed to survive. If not given, many patients may die within days to weeks. For frail, older patients, conservative care (without KRT) may be chosen to maintain comfort and quality of life, even if survival is shorter.
Even patients on KRT, or in earlier CKD stages, often have poor quality of life due to:
- Other chronic conditions (comorbidities)
- Side effects of treatment
CKD and Other Diseases: A Two-Way Street
CKD rarely exists alone. It often coexists with other illnesses like:
- Diabetes
- High blood pressure
- Obesity
These can cause CKD, and CKD can worsen other diseases. Less commonly, infections (HIV, hepatitis) or immune diseases (like lupus) can lead to CKD.
CKD also causes faster aging of the body, especially harming the heart and blood vessels, raising the risk of:
- Heart attacks and strokes
- Heart failure
- Arrhythmias (irregular heartbeats)
- Poor blood flow to limbs
Cardiovascular–Renal–Metabolic Syndrome
CKD, diabetes, and heart disease are closely linked. Together, they form the Cardiovascular-Renal-Metabolic Syndrome. They share:
- Common risk factors (like poor diet and inactivity)
- Similar disease pathways (e.g. inflammation, obesity)
- The need for combined prevention and treatment
Doctors aim to:
- Treat all 3 conditions together
- Screen for one if the other is found
- Recommend lifestyle changes (e.g. walk more, eat fresh food, avoid ultra-processed meals)
Other Serious CKD Effects
- Higher risk of death from any cause (CKD was the top risk factor for COVID-19 death)
- Higher cancer risk (e.g. kidney cancer, skin cancers from immunosuppressants)
- Numerous comorbidities, including:
CKD-related Health Problems & Management
| Problem | Cause | Possible Solution |
| High blood pressure | Salt buildup | Reduce salt, adjust meds |
| Swelling & breathing trouble | Fluid retention | Limit salt, use diuretics |
| Anaemia | Lack of erythropoietin (EPO) | Iron & EPO treatment |
| Bone disorders | Lack of vitamin D | Phosphate control, vitamin D, other meds |
| Malnutrition | Toxin buildup, poor appetite | Nutritional support |
| Nerve damage (neuropathy) | Toxins, diabetes | Manage diabetes and toxins |
| Mental/physical decline | Acidosis, comorbidities | Use bicarbonate |
| Intimacy & pregnancy issues | Mixed causes | Holistic support |
| Depression | Health & lifestyle impact | Psychosocial care |
What Causes CKD?
| Cause | Notes |
| High blood pressure & diabetes | ~50% of CKD in Europe |
| Genetic conditions | ~15%, e.g. ADPKD (kidneys full of cysts) |
| Congenital problems | From birth, e.g. CAKUT (may cause infections, scarring) |
| Glomerulonephritis | Immune-related inflammation of the kidney’s filters |
| Kidney infections | Repeated/severe infections can cause lasting damage |
| Past acute kidney injury | Some never fully recover |
| Unknown cause | Especially common in older adults |
Most congenital/genetic and immune-related cases are considered Rare Kidney Diseases.
Get In Touch
Contact us?